- Ambulatory EKG or ECG. (The terms “EKG” and “ECG” both stand for electrocardiogram.)
- Continuous EKG or ECG.
- EKG event monitors.
- Episodic monitors.
- Mobile cardiac outpatient telemetry systems. This is another name for autodetect recorders.
- Thirty-day event recorders.
- Transtelephonic event monitors. These monitors require the patient to send the collected data by telephone to a doctor’s office or a company that checks the data.
Services Provided
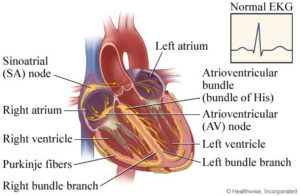
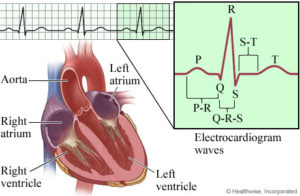
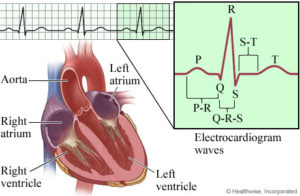
An electrocardiogram (EKG or ECG) is a test that checks for problems with the electrical activity of your heart. An EKG translates the heart’s electrical activity into line tracings on paper. The spikes and dips in the line tracings are called waves. See a picture of the EKG components and intervals .
.
The heart is a muscular pump made up of four chambers . The two upper chambers are called atria, and the two lower chambers are called ventricles. A natural electrical system causes the heart muscle to contract and pump blood through the heart to the lungs and the rest of the body. See a picture of the heart and its electrical system
. The two upper chambers are called atria, and the two lower chambers are called ventricles. A natural electrical system causes the heart muscle to contract and pump blood through the heart to the lungs and the rest of the body. See a picture of the heart and its electrical system .
.
Holter Monitors
Holter monitors sometimes are called continuous EKGs (electrocardiograms). This is because Holter monitors record your heart rhythm continuously for 24 to 48 hours.
A Holter monitor is about the size of a large deck of cards. You can clip it to a belt or carry it in a pocket. Wires connect the device to sensors (called electrodes) that are stuck to your chest using sticky patches. These sensors detect your heart’s electrical signals, and the monitor records your heart rhythm.
Event Monitors
Event monitors are similar to Holter monitors. You wear one while you do your normal daily activities. Most event monitors have wires that connect the device to sensors. The sensors are stuck to your chest using sticky patches.
Unlike Holter monitors, event monitors don’t continuously record your heart’s electrical activity. They only record during symptoms. For many event monitors, you need to start the device when you feel symptoms. Some event monitors start automatically if they detect abnormal heart rhythms.
Event monitors tend to be smaller than Holter monitors because they don’t need to store as much data.
Different types of event monitors work in slightly different ways. Your doctor will explain how to use the monitor before you start wearing it.
Implantable Loop Recorders
You may need an implantable loop recorder if other event monitors can’t provide enough data. Implantable loop recorders are about the size of a pack of gum. This type of event monitor is inserted under the skin on your chest. No wires or chest sensors are used.
Your doctor can program the device to record when you start it during symptoms or automatically if it detects an abnormal heart rhythm. Devices may differ, so your doctor will tell you how to use your recorder. Sometimes a special card is held close to the recorder to start it.
Other Names for Holter and Event Monitors
A stress test, sometimes called a treadmill test or exercise test, helps a doctor find out how well your heart handles work. As your body works harder during the test, it requires more oxygen, so the heart must pump more blood. The test can show if the blood supply is reduced in the arteries that supply the heart. It also helps doctors know the kind and level of exercise appropriate for a patient.
A person taking the test:
- is hooked up to equipment to monitor the heart.
- walks slowly in place on a treadmill. Then the speed is increased for a faster pace and the treadmill is tilted to produce the effect of going up a small hill.
- may be asked to breathe into a tube for a couple of minutes.
- can stop the test at any time if needed.
- afterwards will sit or lie down to have their heart and blood pressure checked.
Heart rate, breathing, blood pressure, electrocardiogram (ECG or EKG), and how tired you feel are monitored during the test.
Healthy people who take the test are at very little risk. It’s about the same as if they walk fast or jog up a big hill. Medical professionals should be present in case something unusual happens during the test.
A physician may recommend an exercise stress test to:
- Diagnose coronary artery disease
- Diagnose a possible heart-related cause of symptoms such as chest pain, shortness of breath or lightheadedness
- Determine a safe level of exercise
- Check the effectiveness of procedures done to improve coronary artery circulation in patients with coronary artery disease
- Predict risk of dangerous heart-related conditions such as a heart attack.
An echocardiogram (also called an echo) is a type of ultrasound test that uses high-pitched sound waves that are sent through a device called a transducer. The device picks up echoes of the sound waves as they bounce off the different parts of your heart. These echoes are turned into moving pictures of your heart that can be seen on a video screen.
test that uses high-pitched sound waves that are sent through a device called a transducer. The device picks up echoes of the sound waves as they bounce off the different parts of your heart. These echoes are turned into moving pictures of your heart that can be seen on a video screen.
The different types of echocardiograms are:
- Transthoracic echocardiogram (TTE). This is the most common type. Views of the heart are obtained by moving the transducer to different locations on your chest or abdominal wall.
- Stress echocardiogram. During this test, an echocardiogram is done both before and after your heart is stressed either by having you exercise or by injecting a medicine that makes your heart beat harder and faster. A stress echocardiogram is usually done to find out if you might have decreased blood flow to your heart (coronary artery disease
 ).
). - Doppler echocardiogram. This test is used to look at how blood flows through the heart chambers, heart valves, and blood vessels. The movement of the blood reflects sound waves to a transducer. The ultrasound computer then measures the direction and speed of the blood flowing through your heart and blood vessels. Doppler measurements may be displayed in black and white or in color.
- Transesophageal echocardiogram (TEE). For this test, the probe is passed down the esophagus
 instead of being moved over the outside of the chest wall. TEE shows clearer pictures of your heart, because the probe is located closer to the heart and because the lungs and bones of the chest wall do not block the sound waves produced by the probe. A sedative
instead of being moved over the outside of the chest wall. TEE shows clearer pictures of your heart, because the probe is located closer to the heart and because the lungs and bones of the chest wall do not block the sound waves produced by the probe. A sedative and an anesthetic
and an anesthetic applied to the throat are used to make you comfortable during this test.
applied to the throat are used to make you comfortable during this test.
- Transesophageal echocardiogram (TEE). For this test, the probe is passed down the esophagus
 instead of being moved over the outside of the chest wall. TEE shows clearer pictures of your heart, because the probe is located closer to the heart and because the lungs and bones of the chest wall do not block the sound waves produced by the probe. A sedative
instead of being moved over the outside of the chest wall. TEE shows clearer pictures of your heart, because the probe is located closer to the heart and because the lungs and bones of the chest wall do not block the sound waves produced by the probe. A sedative and an anesthetic
and an anesthetic applied to the throat are used to make you comfortable during this test.
applied to the throat are used to make you comfortable during this test.
Myocarditis is inflammation of the heart muscle. Myocarditis may occur after a viral, fungal, or bacterial infection, such as diphtheria, rheumatic fever, or tuberculosis.
Treatment for myocarditis includes evaluation and treatment of the cause of the inflammation. Treatment may require use of antibiotics, if a bacterial infection is the cause, and medicines to relieve pain and inflammation. Lifestyle changes, including increased rest and a low-salt diet, may be part of the treatment.
Myocardial Perfusion Imaging, also called a Nuclear Stress Test, is used to assess coronary artery disease, or CAD. CAD is the narrowing of arteries to the heart by the build up of fatty materials.
CAD may prevent the heart muscle from receiving adequate blood supply during stress or periods of exercise. This frequently results in chest pain, which is called angina pectoris. Perfusion imaging usually consists of stress and rest tests.
Images are taken of your heart while at rest and after exercising or under stress. The comparison allows your physician to evaluate blood flow under different levels of exertion. After the images are reviewed, they’ll meet with you to discuss the results.
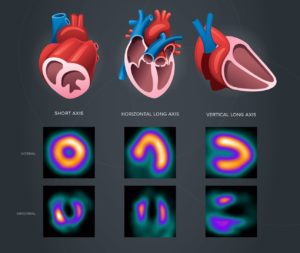
Normal or abnormal, what does it mean?
A normal test result indicates there is sufficient and unrestricted blood flow to your heart, both during periods of rest and exercise. Generally, there’s little concern for coronary artery disease and, in most cases, you won’t require any further testing.
An abnormal result, which means your heart’s blood flow is insufficient, may occur only during the exercise phase of your stress test. During rest, your blood flow may be normal, but during strenuous activity, when your heart is working harder, it may not be getting the blood supply it needs. It’s likely that there is some level of coronary artery disease or blockage.
An abnormal result in both phases of your stress test is an indication that your heart’s blood flow is poor, regardless of your exertion level. The restricted blood flow suggests significant coronary artery disease. If your stress test images show areas of the heart that are not highlighted with the radioactive isotope, it may also be an indication of scar or damaged tissue caused by a previous heart attack.
Regardless of the results, your doctor will explain the findings and address your concerns. If necessary, they’ll recommend a treatment plan that can potentially improve or better manage your heart’s function.
Peripheral vascular disease (PVD) refers to diseases and disorders of the blood vessels outside of the heart, such as those of the brain, gut, kidneys, or limbs. PVD is typically caused by blockage or damage to blood vessels such as veins and arteries.
Think of your body’s circulation like the plumbing in your house: pipes bring water in and take water away. When your heart pumps, blood moves through pipes called arteries to supply all of your organs and limbs. From there, blood returns to the heart in pipes called veins and lymphatic vessels. Each of these vessels can develop its own set of problems.
Over time, arteries can build up with cholesterol plaques and narrow. This can happen to arteries anywhere in the body, for example:
- In the neck arteries that supply the brain, it can cause a mini stroke or a stroke.
- In the arteries to the arms, it may cause fatigue or tiredness in one arm more than the other, or result in a difference in blood pressure between the arms.
- In the heart’s arteries, it may cause shortness of breath, pressure in your chest, arms, neck, back or stomach (in women, the symptoms may be less specific like fatigue or nausea).
- In the arteries to your kidneys, it may cause your blood pressure to be poorly controlled (sometimes suddenly), or may lead to deteriorating kidney function.
- In the aorta, which is the main artery which supplies all organs and limbs, it may contribute to weakening of the wall and formation of an aneurysm, the danger of which is a rupture.
- In the arteries to your legs, it may cause you to start walking slowly and have difficulty keeping up from fatigue, weakness, or discomfort/cramping.
Your veins move blood back to the heart. While veins don’t develop cholesterol build-up, they do develop a very common disease in the legs. To facilitate the movement of blood from the legs to your heart, your veins have valves that allow the blood to flow up to the heart. In some people, these valves may stop working, resulting in blood flowing backward, which is called venous insufficiency.
Symptoms of this disease may include:
- Fatigue or heaviness in the legs, especially at the end of day
- Swelling of ankles
- Cramps at night time
- Itching of skin
- Restless legs
- Pigmentation of skin below the knee
- Formation of visible veins on the legs and sores above the ankle that don’t heal quickly
Peripheral Vascular Disease Management including Angiography, Angioplasty, Atherectomy, and Stenting
Peripheral vascular disease (PVD) refers to diseases and disorders of the blood vessels outside of the heart, such as those of the brain, gut, kidneys, or limbs. PVD is typically caused by blockage or damage to blood vessels such as veins and arteries.
Think of your body’s circulation like the plumbing in your house: pipes bring water in and take water away. When your heart pumps, blood moves through pipes called arteries to supply all of your organs and limbs. From there, blood returns to the heart in pipes called veins and lymphatic vessels. Each of these vessels can develop its own set of problems.
Over time, arteries can build up with cholesterol plaques and narrow. This can happen to arteries anywhere in the body, for example:
- In the neck arteries that supply the brain, it can cause a mini stroke or a stroke.
- In the arteries to the arms, it may cause fatigue or tiredness in one arm more than the other, or result in a difference in blood pressure between the arms.
- In the heart’s arteries, it may cause shortness of breath, pressure in your chest, arms, neck, back or stomach (in women, the symptoms may be less specific like fatigue or nausea).
- In the arteries to your kidneys, it may cause your blood pressure to be poorly controlled (sometimes suddenly), or may lead to deteriorating kidney function.
- In the aorta, which is the main artery which supplies all organs and limbs, it may contribute to weakening of the wall and formation of an aneurysm, the danger of which is a rupture.
- In the arteries to your legs, it may cause you to start walking slowly and have difficulty keeping up from fatigue, weakness, or discomfort/cramping.
Your veins move blood back to the heart. While veins don’t develop cholesterol build-up, they do develop a very common disease in the legs. To facilitate the movement of blood from the legs to your heart, your veins have valves that allow the blood to flow up to the heart. In some people, these valves may stop working, resulting in blood flowing backward, which is called venous insufficiency.
Symptoms of this disease may include:
- Fatigue or heaviness in the legs, especially at the end of day
- Swelling of ankles
- Cramps at night time
- Itching of skin
- Restless legs
- Pigmentation of skin below the knee
- Formation of visible veins on the legs and sores above the ankle that don’t heal quickly
A pacemaker is a small, battery-powered device that sends out small electrical impulses to make the heart muscle to contract. The pacemaker itself is a waterproof object about the size of a silver dollar. A pacemaker consists of a pulse generator and battery that create the electrical impulses, and wires (leads) that transmit electricity to the heart.
Pacemakers help your heart beat in a regular rhythm and at a normal speed. They are inserted to treat a heart rate that is too slow, too fast, or irregular.
Pacemakers are typically placed under the skin of the chest. These pacemakers are permanent. But sometimes, pacemakers are needed for only a short time to help a person in the hospital with heart rhythm problems. A temporary pacemaker is not surgically inserted but is worn outside the body. Temporary pacemakers are used only while a person is in the hospital.
Fast facts
- A tilt-table test involves changing a person’s positioning quickly and seeing how their blood pressure and heart rate respond.
- This test is ordered for people who have symptoms like a rapid heartbeat or who often feel faint when they go from a sitting to standing position. Doctors call this condition syncope.
- Potential risks of the test include nausea, dizziness, and fainting.
Doctors recommend a tilt-table test for patients they suspect may have certain medical conditions, including:
Neurally mediated hypotension
Doctors also call this condition the fainting reflex or autonomic dysfunction. It causes a person’s heart rate to slow down instead of speed up when they stand, which keeps blood from pooling in the legs and arms. As a result, a person may feel faint.
Neurally mediated syncope
A person with this syndrome can experience symptoms such as nausea, lightheadedness, and pale skin, followed by a loss of consciousness.
Postural orthostatic tachycardia syndrome (POTS)
This disorder occurs when a person experiences changes when they suddenly stand up. Doctors associate POTS with an increase in heart rate up to 30 beats and feeling faint within 10 minutes of standing up from a sitting position.
Women between the ages of 15 and 50 are more likely to experience POTS, according to the National Institute of Neurological Disorders and Stroke.
The tilt-table test can simulate the effect of sitting to standing in a controlled environment, so a doctor can see how a person’s body responds.
The purpose of the tilt-table test is for a doctor to view firsthand the symptoms you experience when changing position.
You might not feel ill effects during the procedure, but you may experience symptoms like dizziness, feeling faint, or even fainting. You may also feel very nauseated.
Follow advice on when to eat
Because some people feel nauseated when they go from a sitting to standing position, a doctor may ask you not to eat two to eight hours before the test. This helps to minimize the chance you’ll be sick to your stomach.
Talk about medications you’re taking
Your doctor will also review the medications you’re currently taking and make recommendations about which ones you should take the night before or the morning of your test. If you have a question about a particular medication, ask your doctor.
Consider if you’ll drive yourself or get a ride
You may want a person to drive you home after the procedure. Consider arranging for a ride beforehand to make sure someone is available.
Did you know the human heart beats more than 100,000 times a day? At that pace, it’s no wonder you might feel your heart skip a beat or flutter from time to time. However, if you notice your heart suddenly races or if you have uneven heartbeats that last several minutes, you may have a condition known as atrial fibrillation.
Atrial fibrillation (also called AFib) is a problem with the rate or rhythm of the heartbeat. Your heart’s electrical system tells your heart when to contract and pump blood to the rest of your body. With AFib, these electrical signals short circuit in a sense. This results in a chaotic, rapid heart rate. You might feel short of breath, dizzy and overly tired, although not everyone has these symptoms.
If you have AFib, it’s important to remember you’re not alone. AFib affects more than 3 million Americans. If untreated, it can lead to blood clots, stroke and heart failure. In fact, people with AFib are five times more likely to have a stroke than people without the condition.
As with other heart problems, the choices you make every day can make a difference in your symptoms and general heart health. So, stay in sync with your heart and learn more. Use this condition center to learn more about atrial fibrillation. You can also chat online with other people like you, keep up with the latest research, and get tips to help you feel your best.
Anticoagulant medicines, often called blood thinners, do not actually thin the blood but increase the time it takes a blood clot to form. Anticoagulants help prevent existing blood clots from becoming larger and may be used to prevent deep vein blood clots or to treat certain blood vessel, heart, or lung conditions.
Cholesterol is an important type of fat (lipid) that is made by the body. It is needed for the body to function. It also is found in foods that are made from animal products (meat and dairy products).
Cells need cholesterol to function. But excess cholesterol in the blood builds up in blood vessels and may lead to hardening of the arteries (atherosclerosis), heart disease, and stroke. People who have diabetes are at higher risk for atherosclerosis.
There are two main forms of cholesterol:
- Low-density lipoprotein (LDL) is called “bad cholesterol.” Most efforts to lower cholesterol are aimed at reducing levels of LDL.
- High-density lipoprotein (HDL) is called “good cholesterol.” It can help remove excess cholesterol from the blood vessels.
A person’s cholesterol level can be checked with a blood test.